Signs and Symptoms of Some of the Most Common Eye Diseases
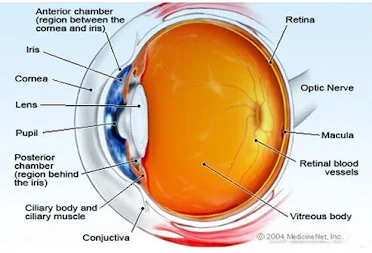
Anatomy of the Eye
The anatomy of the eye is complex. The main structures of the eye include:
Cornea: clear tissue in the very front of the eye
Iris: colored part of the eye surrounding the pupil
Pupil: dark hole in the iris that regulates the amount of light going into the eye
Lens: small clear disk inside the eye that focuses light rays onto the retina
Retina: layer that lines the back of the eye, senses light, and creates electrical impulses that travel through the optic nerve to the brain
Macula: small central area in the retina that allows us to see fine details clearly
Optic nerve: connects the eye to the brain and carries the electrical impulses formed by the retina to the visual cortex of the brain
Vitreous: clear, jelly-like substance that fills the middle of the eye
What Are The Most Common Eye Diseases?
Glaucoma is a group of eye diseases that develop due to elevated intra-ocular pressure (IOP) within the eye. The increased pressure affects the optic nerve and may cause vision loss. Glaucoma is classified either as open-angle (the more common form that is usually painless) or angle-closure glaucoma (which often occurs suddenly and is associated with pain and redness of the eye).
People with a family history of glaucoma, the elderly, and African-Americans are at increased risk of the disease.
Cataracts
A cataract is a painless cloudy lens in the eye that causes blurry vision. It progresses slowly as we age (most people who live long enough will have some cataract-like changes to their cornea). Other causes of cataracts include diabetes, trauma, some medications, and excessive UV light exposure.
Your doctor can see a cataract while doing a routine eye exam. Treatments for cataracts include eyeglasses, magnifying lenses, or surgery. Surgery is curative as the cloudy lens is removed and replaced with an artificial one. The need for surgery and the risks involved should be discussed with your eye doctor.
Age-Related Macular Degeneration (AMD)
Age-related macular degeneration is an eye disease with onset at any age, usually after age 60, that progressively destroys the macula, the central portion of the retina that helps with focus. It rarely causes total blindness as only the center of vision is affected.
There are two types of AMD: wet and dry. In wet AMD, abnormal blood vessels behind the retina start to grow, leaking blood and fluid, causing loss of central vision, which may occur quickly. In dry AMD, the light-sensitive cells in the macula slowly break down causing central vision to diminish over time.
READ ALSO: Eyelashes: Long-Term Effects Of Eyelash Extensions
Retinal Detachment
Retinal detachment occurs when the retina (tissue in the back of the eye) separates (detaches) from its underlying structures. The buildup of fluid behind the retina is what separates the retina from the back of the eye. Retina detachments are often painless, and symptoms that may be noticed include perception of flashing lights, floaters, or a curtain drawn over your visual field. Risk factors for retinal detachment include being a nearsighted adult age 25 to 50, or an elderly person after cataract surgery. Treatment for a detached retina involves surgery, mostly using lasers, that can improve vision affected by the retinal detachment.
Conjunctivitis (Pink Eye)
Conjunctivitis, or pinkeye, is redness and inflammation of the clear tissue covering the eye and the inside of the eyelids (conjunctiva). It is commonly caused by bacterial or viral infections but may also be due to irritants (chemicals, pollutants, or allergens).
Most cases of infectious conjunctivitis are viral and do not need treatment with antibiotics. Bacterial conjunctivitis can be treated with antibiotic drops or ointments prescribed by your doctor. A crusty discharge may make it difficult to open the eyelids. If this happens a warm, wet compress may be applied to the eyes to gently remove the crusting.
To reduce the spread of the infectious conjunctivitis, wash hands frequently, do not share eye drops, cosmetics, towels, or washcloths.
READ MORE: Simple Food Swap Protects Vision as You Age
Uveitis
Uveitis is inflammation to the middle layers of the eye (the uvea). The uvea is the layer of the eye that contains the arteries and veins that feed the important structures used in vision. Causes of uveitis include trauma or injury to the eye, infections, or rheumatologic or inflammatory diseases that affect other parts of the body. The main symptom of uveitis is pain in the eyeball. The eye will look red (bloodshot) and you may notice blurred vision, light sensitivity, and spots in your vision.
Treatment for uveitis depends on the cause. Anti-inflammatory or antibiotic drops, along with pain medications may be prescribed.
Eye Allergies
Severe eye allergies may cause damage to the eye that may threaten eyesight. Allergies can cause chronic inflammation that may permanently damage the cornea. Causes of eye allergies are usually due to seasonal allergies, sensitivities to cosmetics or medications, or dust. Over-the-counter eye drops that contain antihistamines or decongestants are usually helpful. Consult a doctor if OTC remedies do not work, or if you experience pain, discharge, or extreme eye redness.
Sty (Stye)
A sty (also spelled stye) is an infection of the oil gland at the base of an eyelash. It appears as a red, raised pimple on the edge of the eyelid. Symptoms of a sty are pain, tenderness, redness, and swelling with a small pustule. The eyeball itself may feel irritated or as if something is scratching it due to the swelling of the eyelid. Treatment for a sty includes warm compresses applied to the affected area for 10 minutes, up to six times daily.
If the sty comes to a head and releases pus, it should be cleaned gently with soap and water. This rupture usually leads to the sty going away. If the sty is very large, painful, or affects your vision, see your doctor.
Keratoconus
The cornea is the clear surface covering the front of the eye. It is normally smooth and round, following the contour of the eyeball. Weakness in the structure of the cornea can lead to pressure in the eyeball, causing an conical-shaped abnormal bulge to the front of the eye in a condition called keratoconus.
Blepharitis
Blepharitis is inflammation of the eyelids. The inflammation can be found on the outer (anterior) or inner (posterior) eyelid and symptoms include burning, itching, swelling, flaky skin at the base of the lashes, crusting of the eyelids, tearing, or blurred vision. Common causes of blepharitis are problems with oil glands at the base of the eyelids, infections, or other skin conditions.
Chalazion (Eyelid Cyst)
A chalazion (also called a meibomian cyst, tarsal cyst, or conjunctival granuloma) is the inflammation of a small cystic gland in the eyelid. The gland opening becomes clogged and the gland swells. Chalazia are treated with warm compresses, though in rare cases they may require antibiotics. If the chalazion becomes severe, causes changes in vision, or is persistent, it may be removed surgically.
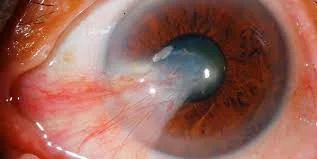
Corneal Ulcer
A corneal ulcer is a small crater (ulcer) on the front part of the eye, usually resulting from infection. Bacteria, viruses, or fungus can cause a corneal ulcer. People who wear contact lenses are at higher risk for corneal ulcers because infectious agents may get trapped behind a lens. Symptoms of a corneal ulcer include pain, intense redness, feeling as if the eye is scratched or something is in the eye, sensitivity to light, and blurry vision. If you suspect a corneal ulcer or have the symptoms of a corneal ulcer and wear contact lenses, see your ophthalmologist immediately. High potency antibiotics and pain medications are the treatments for this condition.
Diabetic Retinopathy
People with diabetes often have problems with their blood vessels throughout their bodies and the eye is no exception. A complication of diabetes is diabetic retinopathy, which affects the blood vessels in the back of the eye, on the retina.
There are two types of diabetic retinopathy:
Nonproliferative retinopathy: the less severe type in which there may be bleeding in the retina and leakage of blood or serum causing a “wet retina.”
Proliferative retinopathy: a more severe type where new abnormal blood vessels grow on the retina. These vessels may bleed into the vitreous (the clear jelly in the center of the eye) and cause visual problems.
Treatment involves laser surgery but damage may be permanent. The best way to prevent diabetic retinopathy is with strict glucose control and a healthy lifestyle (weight loss, dietary restrictions, and exercise).
Strabismus (Crossed Eyes)
Crossed eyes (strabismus) is a condition where the eyes do not look in the same direction as they should. One eye may track differently than the other causing a disjointed appearance. Young children born with this disorder may develop decreased vision in one eye (amblyopia).
Floaters
Floaters are caused by aging changes in the vitreous jelly of the eye. They are a common consequence of aging. If you develop multiple floaters, or floaters associated with pain, get checked by your ophthalmologist. In general floaters do not cause blindness and are mostly harmless. There is no definitive treatment for floaters, as most will fade or become less noticeable over time.
Farsightedness (Hyperopia)
Farsightedness (hyperopia) is difficulty focusing on objects that are close. It is very common and the incidence increases with age. It is caused by an abnormally flat cornea that does not allow light to sharply focus on the retina.
Nearsightedness (Myopia)
Nearsightedness (myopia) causes people to be unable to see distant objects, though they can see nearby objects clearly. It is caused by the cornea having too much curvature, resulting in problems with focusing on the retina. Myopia is extremely common and easily corrected with eyeglasses, contact lenses, or surgery.
Astigmatism
Another common cause of visual difficulty is astigmatism, in which images are blurred due to an irregularly-shaped cornea. Astigmatism will eventually affect most people as a part of the aging process. It is treated with glasses, contact lenses, or refractive laser eye surgery.
Color Blindness
The colors we see are a result of how our eyes (and thus our brains) interpret different wavelengths of light. People with color blindness have difficulty seeing certain colors, usually reds, greens, and blues. Color blindness is caused by an absence or malfunction of color-sensitive cells located in the retina. Most of the time this is genetic (people are born with it) but it can also be caused by aging, disease, trauma to the eye, or certain medications. If the cause of the color blindness is genetic, the problem cannot be corrected but people may be trained to adapt to interpret color shades. In cases where color blindness is acquired, it may be treatable.
READ ALSO: 8 Wonderful Health Benefits Of Beetroots
Proactive Eye Health
Take care of your eyes to protect your vision. Always use eye protection to avoid injuries and wear sunglasses to protect your eyes from UV rays. People over 40 should have their eyes checked every two years and people over 60 should have their eyes checked every year.
Be proactive in your eye health. If you notice any symptoms of the disorders discussed in this article, see your ophthalmologist.